Tēnā koutou katoa
Well, winter has arrived! It was sleeting as I drove to work yesterday, and I am sure many of you are looking out to snow today. So I’m very pleased to be able to announce that WellSouth will be funding Winter Wellness Checks for eligible people starting Monday week. We will have more detail to follow next week but there is a summary of the concept here.
You will have also seen the announcement from Minister Verrall regarding extra services for eight areas around Aotearoa over the winter months, one of which is Invercargill. The details of what this means on the ground have yet to be determined. As soon as we know more from Te Whatu Ora, I will pass that information on.
Key points today:
-
Winter Wellness Checks starting soon
-
New report shows Tōku Oranga – Access and Choice programme making a difference, service is equitable
-
New community-based alcohol and drug addictions service launches in Otago
-
Localities Update
-
Cilazapril Reminder
-
ESR Risk Assessment
-
Welcoming WellSouth Clinical Nurse Advisor/Leader
-
Building the future of health hui recording
-
Who’s who of primary care atop the new health system – NZ Doctor 09 May 2023
-
Privacy Week 2023
-
Understanding blood cancers and condition in primary health – Survey
-
Wānanga Tōkeke: Equity in Health Workshop - Invercargill
-
Assisted dying – Canterbury Initiative education webinar
-
Southern Eating Disorder Service
-
Introducing more of our clinical advisors
-
Covid-19 update
What’s new
Winter Wellness Programme
WellSouth wants to support practices help patients and whānau – particularly those most at risk of getting very unwell during winter.
A new Winter Wellness Check will fund General Practice to proactively contact and provide an additional routine and preventative care for patients who are at risk of deteriorating or being admitted to the hospital over the winter months, and ensure they have what they need to stay well.
This pilot programme will run 22 May to 30 June, so that patients can best benefit before Winter sets in.
More detail will follow next week, however, some of the key points:
-
Each practice will be allocated a number of Winter Wellness claims based on the eligibility criteria applied to their practice population.
-
You, as a practice, will select who of your eligible patients you would like to invite to participate, based on eligibility criteria:
|
These people: |
With one of these health conditions |
|
Māori |
Asthma |
|
Pasifika |
Cardiovascular Disease |
|
Former Refugee |
COPD |
|
Live in a Quintile 5 area |
Heart Failure |
|
Community Services Card holder |
Severe enduring mental illness |
|
|
Diabetes with latest HbA1c >= 64 mmol/l |
-
We will provide further guidance on the components of the Winter Wellness check with the patient, which in broad outline includes an in-person
-
Check that relevant vaccinations are up to date, and offer if not
-
Medication review
-
Personal Action Plan for the patient promoting self-management of conditions
-
Back pocket scripts, as appropriate
-
Update/create the acute plan in HealthOne
-
-
The fee paid to the practice for each claim will be $100 + GST.
We anticipate that this will largely be a nurse-led process, with general practitioner or nurse practitioner input as required.
We understand that capacity is a major issue across practices and that winter illnesses can exacerbate challenges. Our aim is for these checks to enable preventative care and help reduce acute workload for practices over winter, as well as improving people’s experience. Further information will be coming through next week.
New report shows Tōku Oranga-Access and Choice programme making a difference, service is equitable
WellSouth commissioned an independent research report on the Tōku Oranga – Access and Choice programme to determine whether the programme is meeting the needs of the community and to identify how it could improve.
The reports describes the impact of the service delivered through general practices across Southern as having meaningful and measurable benefits for patients.
Evaluation of the Tōku-Oranga-Access and Choice Programme report finds there is ‘evidence of the programme’s effectiveness’, including ‘significant improvements in mental, physical and social health for patients.’
As for areas of improvement, consulting group Synergia suggests more people need to know about the service -- and know they can self-refer to access support.
Read the summary, evaluation report and full news release here.
New community-based alcohol and drug addictions service launches in Otago
A new Kaupapa Māori service for people with complex AOD (alcohol and other drug) needs including current or past corrections histories.
The service is available to all adults who seek support in their recovery, including those with current and/or past involvement with Corrections. The new services will have an expert workforce who will be culturally safe and confident with providing support services to Māori and Pasifika.
Tāngata whaiora (a person seeking health) and their whānau will experience an open-door-whare steeped in Te Ao Māori, where kaimahi warmly manaaki them into an environment that caters to their recovery needs.
Participants will have the benefit of clinical outpatient services, outreach services with wānanga, whānau ora approaches, therapeutic interventions, and peer support delivered within a Te Ao Māori framework. Tāngata whaiora will also be able to connect directly with the other Te Kāika services to receive he korowai manaaki (a cloak of care and support).
The service can be accessed in the following ways:
- Tāngata whaiora can self-refer
- Referral by whānau
- Referral by GP
- Referral by other external parties
Those requiring the service, or wanting to refer whānau into the service, can express interest at tewhare@tekaika.nz
Localities Update
Hokonui submitted their draft locality plan to Te Whatu Ora on 28 April, derived from a robust community engagement process and discussion with the Iwi-Māori Partnership Board (IMPB) and Te Aka Whai Ora. Four themes came from the engagement: access, cost of living, mental wellbeing, and the psycho-social effects of the pandemic. These consequently gave rise to the five priorities below. The locality group's main goal now is to show to the local community that change has come about as a result of the engagement process (they are due to work with the regional commissioner in May/June on service development). The community is updated via a monthly section in the local newspaper, social media, and www.hokonuilocality.nz
The national rollout process for other localities is now underway, with the first step being the IMPB’s recommendation for boundaries to Te Whatu Ora (this is pending), then consultation with local government (Councils are being informed about this process over the coming months), then a draft determination by Te Whatu Ora and community consultation on this. We understand Te Whatu Ora is working towards releasing the draft boundaries in in the latter part of this year.
WellSouth continues to support communities and providers with guidance regarding localities. The key message for other parts of Otago Southland at present is the national process is in train and to wait for these processes.
Hokonui Priorities
-
Connection, navigation and ease of use: The voice of the community has clearly asked for services to be developed that are in fact available, engaged and suit community usage. Our community is seeking active treatment plans with regular updates and complementary wraparound services.
-
Information and communication: There needs to be much clearer, obvious and locatable communication with community about the type of help that is available and how to access it. This will make getting the right help quicker and easier and will help us look after ourselves and our families.
-
Oral health: There needs to be a major re-think about dentistry in Hokonui, including immediate work on waiting lists, longer-term planning to ensure ongoing provision, and a focus on prevention.
-
Experiencing respect and compassion: We feel confident accessing health services and feel heard and respected. Providers feel confident and are equipped and supported to deal with our mental, spiritual and whānau health. Community receives quality and equitable services without needing advocacy. Reduced acute cases as the public will access medical care earlier in illness.
-
Community inclusivity: We think more effort going into creating and supporting inclusive community events and activities will reduce stress, anxiety, and loneliness, and increase resilience and community pride. Looking after natural and built environments is also really important as much of what we want to do starts with having a cleaner healthier environment, in particular the Mataura River.
Cilazapril Reminder
Our team have been visiting practices to remind them to transfer patients off Cilazapril as the supply will end soon and it will not be available again.
We have had practices report that all their patients have been switched, but when we review the patient data there are still patients on Cilazapril.
There are a few reasons this may happen including;
-
repeat prescriptions though Manage My Health putting more Cilazapril scripts through, or repeat all in the PMS.
-
patient’s not wanting to change from Cilazapril (but eventually they will have to, as Cilazapril won’t be there)
-
and in some instances, another clinician putting people back onto Cilazapril
If patients remain on Cilazapril when the supply ends, they will end up with a prescription that can’t be filled.
To avoid disruption for your patients and practice we encourage you to review your patients and switch them off Cilazapril as soon as possible.
You can use Thalamus to check who you still have on Cilazapril (if you need assistance with Thalamus, contact Glen or Susie via glen.knol@wellsouth.org.nz or susie.lawless@wellsouth.org.nz)
ESR Measles Risk Assessment – very high public health risk
A message from ESR:
The latest ESR risk assessment puts the likelihood of transmission within New Zealand as moderate to high. Given the lower than optimal childhood immunisation rates in New Zealand, the known measles immunity gaps in the young adult population, as well as the highly infectious nature of measles, the likelihood of limited localised transmission from an imported case is high.
There is also a moderate likelihood of larger localised outbreaks with the potential for a widespread epidemic within New Zealand, similar to that seen in 2019 if local cases are not detected and managed rapidly.
The overall public health risk is very high. If measles transmission were to become established in New Zealand, the overall public health impact would be very high given the impacts on people and the health sector nationally and the potential loss of New Zealand’s measles elimination status.
So please, continue to prioritise and fund childhood immunisation and particularly focus on strategies that reduce the inequities in coverage. Travellers should also ensure they are fully vaccinated before travel.
Welcoming WellSouth Clinical Nurse Advisor/Leader
We are delighted to welcome Kate Norris to WellSouth, in the newly created role of Clinical Nurse Advisor/Leader.
Kate has more than 30 years experience in nursing and is a keen advocate for nursing education and training. She is based in Wanaka and will support practices throughout the region.
Like the rest of the WellSouth team, Kate sees huge opportunity in the health system reforms and is keen to be part of making sure primary and community care nurses have more and better opportunities to make meaningful change.
I know Kate plans to be in touch directly tomorrow (Happy International Nurses Day!) but I wanted to welcome my colleague and I look forward to the benefit of her clinical input and leadership.
You can contact Kate at kate.norris@wellsouth.org.nz

Building the future of health hui recording
Te Whatu Ora and Te Aka Whai Ora held their latest stakeholder hui on 3 May 2023.
The recording is available here.
In this hui:
-
Updates were provided by special guests, Naomi Ferguson, Chair of the Board, and Dr Diana Sarfati, Director-General of Health and Chief Executive of Manatū Hauroa.
-
Riana Manuel, Chief Executive of Te Aka Whai Ora and Margie Apa, Chief Executive of Te Whatu Ora also supplied updates on their respective programmes of work.
-
Our guest speakers, Aroha Metcalf and Jo Chiplin shared some of the mental health mahi underway and the rollout of some exciting new initiatives.
For those who were unable to attend or if you would like to recap please go to the stakeholder pages of the Te Aka Whai Ora and Te Whatu Ora websites to view the recording.
If you’d like to review all previous hui and questions, you can find them here: Stakeholder Hui – Te Whatu Ora - Health New Zealand
Who’s who of primary care atop the new health system – NZ Doctor 09 May 2023
A few short bios of people important to primary care at national level in the health system.
Read the article attached here.
Republished with permission of New Zealand Doctor Rata Aotearoa.
Privacy Week 2023
It is Privacy Awareness week, and we want to take this opportunity to highlight the significance of privacy rights and the importance of protecting patient information within the primary care sector.
This annual event, organised by the Office of the Privacy Commissioner, serves as a reminder of our responsibility to safeguard patient privacy in this digital age.
The Privacy Commissioner website have free eLearning courses to help understand Privacy codes and best practices which may be useful for your staff to complete if they are new or as a refresher.
Health ABC is designed for busy health and disability workers who only need the basics of health information privacy. It takes less than an hour to complete and uses scenarios to bring concepts to life. It’s also divided into 12 short sections, so you can easily dive into the information you need, when you need it.
Health 101 will introduce you to key concepts and definitions contained in the Health Information Privacy Code (HIPC) and how they may be applied in practice. The training takes approximately 3-4 hours but does not have to be completed in a single session.
Opportunities to be involved
Understanding Blood Cancers and Conditions in Primary Health – Survey
Short survey (two minutes) - https://www.surveymonkey.com/r/Understandingbloodcancersandconditionsinprimaryhealth
There are an estimated 21,000 people living with a blood cancer or blood condition in New Zealand, and every day 8 children and adults receive a new diagnosis. Most of these people will be involved with primary health services at some point – particularly those with chronic conditions, or those under active monitoring.
Leukaemia & Blood Cancer New Zealand is the leading organisation dedicated to supporting patients and their whānau living with blood cancers and conditions, and they are teaming up with haematologists from around New Zealand to provide quality educational webinars to upskill primary health professionals (GPs, practice nurses, district nurses etc) on early detection and diagnosis of blood conditions, as well as equipping practitioners to manage these patients in their care and in the community.
To guide them in the planning and delivery of these webinars, and to ensure your knowledge needs are being met, they would greatly appreciate your completion of this short two minute survey.
Upcoming training and webinars
Wānanga Tōkeke: Equity in Health Workshop – Invercargill
Date & time: Thursday 25 May 2023, 5 – 8pm
Location: Invercargill
Register: https://wellsouth.arlo.co/register?sgid=49edf24047a743c79b015f77ba29eaa2
Join WellSouth’s Pou Tōkeke Māori, Riiti Conway (Tuvalu, Kiribati) and Pou Tōkeke, Emma-May Loretz (Ngāi Tahu, Ngāti Tamaterā) to learn about:
-
Mihimihi & pepeha
-
Foundations of Te Ao Māori
-
Equity in General Practice
-
Decolonising Primary Care: Overview of Cultural Safety and Cultural Competency
This workshop is open to anyone working in Primary Care, and will provide you with a general understanding of the above topics while helping you honour your obligations to Te Tiriti o Waitangi and present you with some practical skills that you can take into your practices.
If you have any queries about the workshop, or if you would like to organise a date for your whole practice to complete, please email workforce@wellsouth.org.nz
Assisted Dying – Canterbury Initiative Education Webinar
Date & time: Tuesday 23 May 2023, 7 - 8pm
Location: Online - Zoom webinar
Register: https://tinyurl.com/CIAD2305
Assisted Dying (AD) became legal in New Zealand with the passing of the End of Life Choice Act 2019. Regardless of one’s personal view, healthcare practitioners have specific obligations under the law and need to understand the legislation and know how to respond.
This webinar aims to provide clarity around these obligations and will also discuss how assisted dying is operating in practice New Zealand wide and Canterbury specifically.
The session has been endorsed by The Royal New Zealand College of General Practitioners (RNZCGP) and has been approved for up to 1 CME credits for Continuing Professional Development (CPD) purposes.
Topics for discussion include:
-
Overview of the Act and service, including national data
-
Responding to requests
-
clinician responsibilities
-
practice or service responsibilities
-
-
Referral pathways
-
Clinician perspectives of Assisted Dying in practice
The webinar will include presentation followed by moderated questions and answers via Zoom Q&A. You can submit questions during the webinar or via the Questions & Comments field in the registration form.
The session will be recorded and made available on Canterbury Community HealthPathways.
See the event poster for further information.
Other general information
Southern Eating Disorder Service
The Southern Eating Disorder Service (SSEDS) is a community-based eating disorder service based in Dunedin that covers the Southern geographical region (Waitaki, Otago, Southland, and Central Otago), and operates under the Governance of Ashburn Clinic.
The SSEDS provides early identification, brief intervention, evidence-based treatment, and recovery-orientated community services for people requiring support for disordered eating and eating disorder issues.
GPs can refer to the service, please review the Information sheet for clinicians for further details on how to refer, the referral process to SSEDS can be found on HealthPathways.
For more information on the service including eligibility and the referral process please see the resources linked below.
Information sheet for clinicians
Information sheet for clients and their whānau/family and friends
Introducing our clinical advisors
This week we are introducing two more of our clinical advisors at WellSouth. Please feel free to contact them when you have an issue or idea relating to their areas.
Dr Richard Macharg FRNZCGP, Clinical Advisor
WellSouth Clinical Lead for the Southern Fracture Liaison Service, GP Referred MRI Programme and Concussion Management Pilot
I have been working for WellSouth since last year, now leading the above projects, run by WellSouth with ACC funding. I believe strongly in the value of all of these to our patients here in the South.
Originally from Scotland and qualifying in Aberdeen, I have spent the vast majority of my practising life here in Otago/Southland having arrived in 1988 as a house surgeon. I spent 10 years in Invercargill with hospital time as an Orthopaedic registrar, 15 months in Paediatrics and a diploma in O+G before GP training and a subsequent 5 years as a GP in Don Street and at the Alliance Lorneville plant! I was then a full time GP in Queenstown for many years with snow sports and mountain biking continuing to keep me busy at work and play. I have been a long-term practice owner and at various times a managing director and CEO of a large medical centre and led Cornerstone and more recently, Health Care Home accreditation. I have been a GP teacher and supervisor an ACC GPSI and am a firm believer in the work of specialist general practitioners. I have tried to contribute positively at a regional level and been involved in many discussions around models of care in rural and “isolated urban areas” regionally and nationally. A contribution to rural funding allocation discussions brought my first and very positive experience of WellSouth’s role and I am keen to continue to contribute positively with projects that bring value to patients through best use of care.
Richard.Macharg@wellsouth.org.nz

Dr Kim Hurst, Clinical Advisor
I am excited to be the newest recruit at WellSouth. I am a General Practitioner, keen cyclist, wife, and mother on two young boys. I was born in the UK and spent much of my childhood in rural Mid Wales. I studied at the University of Birmingham before joining the Royal Air Force in 2002. I completed my General Practitioner training in the military, which gave me experience delivering primary care in a variety of environments, from the Scottish Highlands to Kosovo. In 2009, I moved to New Zealand and worked and lived in the Hutt Valley until 2022. During that time, I had a busy life combining general practice with working for Te Awa Kairangi PHO as a Clinical Director. Last year, my family and I relocated to Central Otago, where I intend to see out the next 20 years of my career. I am excited to work in this role for WellSouth because I am driven by advocating for the incredible mahi we all do collectively as primary care providers, as well as helping us all bring our best game.

Covid-19 updates
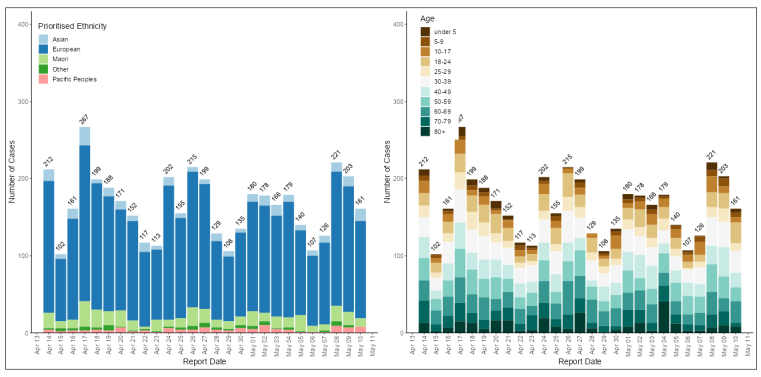
Southern Numbers
Reported Covid cases continue to bubble along at a similar rate for the last few weeks, as shown below:
What beyond the end of June for Covid funding?
That is a good question! The answer to that is not yet clear, and central health agencies are working on figuring that out at the moment. As I understand it, any plans need Cabinet approval, and hopefully things will be clearer after the government budget. But if past behaviour is the best indicator of future behaviour, those timelines may be optimistic.
So on that cheerful note, I’ll sign off! I hope you have a relaxing weekend, and we will be in contact next week with detailed information about the Winter Wellness Checks.
Ngā mihi nui
Carol